COVID-19 took the lives of many elderly adults. Even with the protection of those initial vaccinations for those over 65, the risk of dying from COVID-19 was 60-fold greater than for an individual aged 18-30; for those 75 or older, the risk of death was 140=fold greater. Why might this be? Is it all due to frailty, the lack of resilience that comes with age? A study of the unvaccinated and hospitalized points to an aging and increasingly dysfunctional immune response.
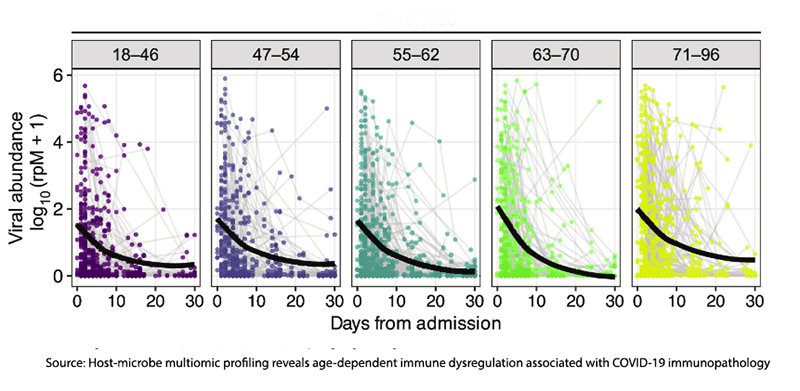
The study analyzed data from 1031 unvaccinated adults hospitalized with COVID-19 who were part of the IMPACC (IMmunoPhenotyping Assessment in a COVID-19 Cohort). They collected blood and nasal swab samples from these patients at up to six visits, starting from admission to the hospital. The participants were divided into age groups, and the trajectory of disease, “from mild disease with brief length of hospital stay … to severe disease and death.” Advancing age was associated with more severe disease and death.
Using a variety of techniques, the researchers characterized
“…the impact of aging on SARS-CoV-2 viral relative abundance, anti–SARS–CoV–2 antibody (Ab) titers, host gene expression, inflammatory protein expression, immune cell populations, and the nasal microbiome.”
The elderly had
- Higher COVID-19 abundance, with lower antibody titers and impaired viral clearance, manifested over the course of their illness rather than at symptom onset.
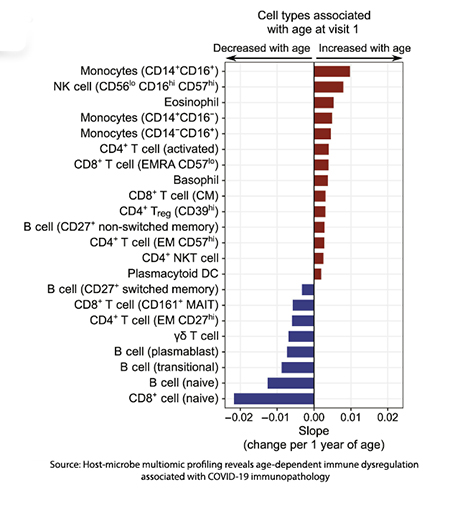 Differences in immune cell populations compared to younger patients, more specifically lower proportions of cells “ which contribute to the effective clearance of viral pathogens.”
Differences in immune cell populations compared to younger patients, more specifically lower proportions of cells “ which contribute to the effective clearance of viral pathogens.”- The expression of genes associated with these immune cell populations are age-dependent. Some pathways are up-regulated, others downward. This was partly due to the greater viral load on admission among the elderly, but over the course of hospitalization, gene expression resulted in “both greater activation and impaired attenuation of immune signaling with advanced age.”
- Significant increases in several cytokines and chemokines immune signals demonstrated a continued coordinated, but now dysfunctional, immune response.
Our Immune Dance
It would be helpful to think of our immune response, not in the isolation of antibodies and T cells but in a coordinated “dance” over time. Beginning with detection and an early, robust innate immune response, a “call to arms” to our adaptive immune system, and with the effective control of, in this instance, COVID-19, a return of the immune system’s inflammatory response to its baseline preventing “excessive tissue damage and pathologic consequences.”
Aging brings dysfunction to the individual steps as well as their coordination, creating, as the authors write,
“age-dependent dysregulation of this program at the transcriptional, protein, and cellular levels, manifesting in an imbalance of inflammatory responses over the course of hospitalization. Our results identify discrete innate and adaptive immune signaling pathways that are altered with age.”
From a more clinical view, the prolonged dysfunctional inflammatory response of severe COVID-19, e.g., cytokine storms, is a frequent dysfunction seen in the elderly patients in this study. The researchers note that this may open the door to more age-specific immunomodulatory therapies directed at this age group's differing cytokine and cellular responses.
Source: Host-microbe multiomic profiling reveals age-dependent immune dysregulation associated with COVID-19 immunopathology Science translational medicine DOI: 10.1126/scitranslmed.adj5154




