 In terms of public perception, drug companies rank in the general vicinity of ringworm.
In terms of public perception, drug companies rank in the general vicinity of ringworm.
Some of this is warranted (especially when companies fudge or withhold safety data), but much is not. We hear the negative constantly, and the positive very rarely.
Much of this is based on a long-running script used by politicians and others looking to score points, as well as media bias and incomplete information, for example, the following.
A new report by IMS Health, a consulting company that provides information and analyses of multiple facets of healthcare economic, scientific, others concluded that prescription drug costs jumped by more than 13 percent last year the biggest increase since 2001.
The company collects data and analyses of sales of pharmaceutical products, which are essential for establishing trends in current and future research, productivity, and economic impact in the world of drugs.
At first glance, the report s headline implies that this is just one more of the many damning criticisms price gouging of the industry that we hear about regularly. But a more careful look at the report reveals something quite different.
Of the $43 billion increase in US spending on pharmaceuticals, almost one-third was a direct results of the first effective hepatitis C drugs hitting the market. The $12.3 billion spent on combatting this infection cannot be lumped in with the other increased expenditures, because the long-awaited availability of these new drugs will probably decrease the future cost of prescription drugs, and other medical costs as well.
ACSH s Dr. Josh Bloom, who spent much of his career doing hepatitis C (HCV) research, explains: In a sense, the huge increase of the cost of HCV expenditures can be looked at as a one time event. The entire landscape of the management of this infection has changed, and this will eventually save not only lives, but money as well.
How can this be? There are several reasons.
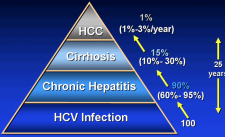
Dr. Bloom explains, First of all, the new drugs, although very expensive, will be used only once per patient. Between 90-100% of HCV-infected patients will be cured. This is not a chronic treatment, such as with HIV/AIDS. For every person cured, there will be one less person to treat. This is borne out by the 10-fold increase in HCV treatment between 2013 and 2014. About 160,000 patients began treatment in 2014 (as compared to 17,000 in 2013). This number represents about five percent of the total of all infected people in the US.
There are less obvious cost savings that will certainly result from the increased use of these drugs. First, HCV is the number one cause of liver transplants in the US. Since a liver transplant costs about $1 million, there is an obvious cost-saving benefit right there.
Also, explains Dr Bloom, There were significant costs associated with the former (and now obsolete) regimen to combat the infection. Not only was interferon-ribavirin the previous standard of care very difficult to tolerate because of severe side effects, but a course of these drugs cost about $30,000 and required a treatment period of between six and 24 months. And it only worked about half time. The new drugs make those in the previous regimen look like something from the Middle Ages.
The interval between the beginning of HCV research and the launch of the first really good drug was 24 years, during which time the only "results" were one failure after another, along with an incalculable expense. Virtually every drug company was doing HCV research, and so far, only two have successful drugs.
Dr. Bloom concludes, This is a once in a generation pharmaceutical breakthrough, and will eventually wipe out most of an infection that plagues 3 million people in the US, and 170 million worldwide. Some things are really worth paying for. This is one of them.


