
Person-centered counseling is one of the most popular treatments for mental health problems. Often just shortened to “counseling”, the approach focuses on how patients view themselves in the here and now, rather than how a therapist interprets their unconscious thoughts. And the patient takes the lead in finding solutions to their own problems.
This “humanistic” form of therapy was developed by Carl Rogers in the 1940s and is now one of three main mental health treatments, alongside cognitive behavioral therapy (CBT) and psychodynamic therapy. However, despite its popularity and longevity, counseling doesn’t appear to make people better in the long term.
Mental health issues are a huge global problem. The World Health Organisation estimates that between 35% and 50% of people in developed countries suffer from anxiety or depression in any given year. And the cost of treating these conditions is enormous – about $2 trillion – so knowing what works and what doesn’t is critical.
Mounting evidence
In 2003, a review of clinical trials showed that counseling provides short-term, modest improvements in reducing anxiety and depression, compared with “usual care” (routine visits to a GP, CBT and antidepressant drugs), but no long-term improvements.
A more recent review, by the highly respected Cochrane organization, investigated whether counseling was effective for mental health and “psychosocial” problems or “problems in living”. The analysis of nine trials showed that counseling was more effective than routine visits to the GP, in the short term (one to six months). In the long term (seven to 36 months), though, it was no longer as effective. Counseling also failed to have an impact on patients’ short or long-term social functioning, such as work, leisure activities and family relationships.
The authors of the review also looked at cost effectiveness. They found that counseling did not reduce overall health costs, and, in some instances, may have increased them.
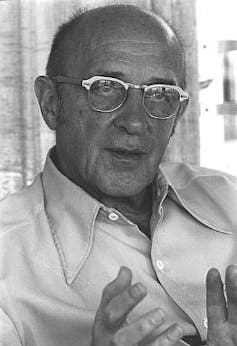
Carl Rogers, the father of counseling. Wikimedia Commons
The biggest randomized trial of its kind to date (755 participants) recently compared acupuncture with counseling in the treatment of depression. Consistent with previous findings, both counseling and acupuncture showed small to moderate levels of effectiveness compared with usual care, up to six months after treatment. But the effects of both treatments were no better than usual care at seven months and beyond. This finding calls into question the long-term benefits that these two treatments offer above and beyond just visiting a doctor.
The picture is the same for younger age groups. School children who received counseling for psychological distress fared better at six weeks than those on a waiting list for treatment. But at 12 weeks there was no real difference between the groups.
Back to the drawing board
Often researchers and practitioners of counseling argue that randomized control trials are too rigid and don’t truly reflect what happens in counseling practice. But a study that evaluated data from UK counseling services, found that, in a sample of 26,527 people with depression, 53% did not make any reliable and clinically significant improvement in their symptoms after receiving a course of counseling. Unfortunately, no follow up data exists on whether the minority who improved, benefited in the long term.
Based on the best evidence available, it appears that counseling is only a short-term strategy for tackling mental health issues. After nearly 80 years, only a small number of empirically robust studies exist, and findings indicate that long-term effectiveness is no better than a non-mental health based intervention, such as seeing a GP.
This brings into question the cost effectiveness of this approach. If no long-term gains are made, we end up with a revolving door syndrome where patients repeatedly relapse and have to have more rounds of treatment. Not only does this drain healthcare resources, it also diminishes patient hope.
As counseling has no impact on social functioning, such as work and family relationships, it has wider personal and economic implications for patients and services.
For any form of therapy to be effective in the long term, it must have a robust and well-supported theory on which to base its treatment. Counseling works on the premise that the therapist must provide key conditions for a patient to achieve personality change, in particular: empathy, genuineness and unconditional acceptance. Unfortunately, the theory also lacks sound evidence and benefits of some of these traits, such as empathy, have been called into question.
 For counseling to help those suffering from mental health issues, its advocates will need to revisit the underlying theory. In the mean time, mental healthcare resources should be reallocated to therapies that have been proven to be effective in the long term, such as CBT.
For counseling to help those suffering from mental health issues, its advocates will need to revisit the underlying theory. In the mean time, mental healthcare resources should be reallocated to therapies that have been proven to be effective in the long term, such as CBT.
By Robin Bailey, Seniour Lecturer in Psychological Therapies, University of Central Lancashire. This article was originally published on The Conversation. Read the original article.


