There has been a lot of confusion in regard to possible treatments for COVID-19 and the timeline for the development and deployment of those treatments. To clarify, we first need to define what we mean by "treatment," because there are a wide variety, including vaccines, antivirals, and antibodies.
Vaccines
A vaccine won’t be available for at least a year or two. (Also, a vaccine may or may not work.) The reason is because vaccines must be tested scrupulously for safety. An article written by Derek Lowe in Chemistry World goes into more detail, but the gist is this: A vaccine is given to millions – perhaps billions – of healthy people, including children. We have to be darn sure that what we’re injecting into people is safe and actually works. There are horror stories of children dying from poorly designed vaccines. Even under the best of circumstances, vaccines can trigger mildly unpleasant side effects (e.g., sore arm) or even rare fatal autoimmune conditions. (No, they still don't cause autism.)
Antivirals
For that reason, most likely, an antiviral will be available before a vaccine. Because drug discovery is a long and arduous process, the best hope we have right now is to repurpose an existing drug. Essentially, we’re taking drugs off the shelf and seeing if they work to treat COVID-19. The drug that is currently generating the most excitement is called remdesivir. It was originally designed to treat Ebola. (It didn’t work.)
However, there are good reasons to believe it may at least help patients infected with coronavirus. Gilead, the drug’s maker, has already launched Phase III clinical trials. These trials should wrap up in April or May. If they end up being successful, a decent supply could be ready by the summer.
Antibodies
Other treatments that are in development include antibodies. These can do various things, depending on what they bind to. One strategy is to use antibodies that have an anti-inflammatory effect. These won’t “cure” the virus, but they can help tame an overreactive immune response, such as a cytokine storm, that could be playing a role in the critical cases of COVID-19. Genentech has launched a Phase III clinical trial of an antibody (originally developed to treat an autoimmune condition called rheumatoid arthritis) that may help.
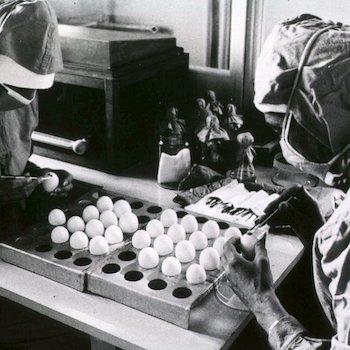
Another strategy is to develop neutralizing antibodies, such as those found in the blood plasma of people who successfully fought off an infection. These bind to the virus and prevent infection. Dr. Jacob Glanville claims that, if all goes according to plan, he could develop a supply of antibodies by September.
How Effective Will the Treatments Be?
We won’t have a good idea of that until we start seeing clinical trial data. “Success” can be measured in various ways (not just preventing death). Researchers also look for outcomes such as improvement of clinical symptoms or improvement of hospital discharge rates. Getting people home faster is obviously important when hospitals are overwhelmed with patients.
Will Treatment Eliminate the Disease?
Probably not. The virus will be with us for the foreseeable future. It’s not even clear if a vaccine will make the disease “go away” because there is evidence that humans do not develop long-lasting immunity to coronaviruses. That doesn’t mean a vaccine would be useless. It just means that, if a vaccine works, we may need to get frequent booster shots. Partial immune protection is still better than none.