A recent article, “A new, lower threshold for lead poisoning in children means more kids will get tested – but the ultimate solution is eliminating lead sources,” talks about an important change in CDC guidance regarding children’s blood lead levels. While the headline is a bit misleading, a new threshold will not ensure more testing; the substance is very important.
What is the CDC Blood Lead Reference Value?
The CDC blood lead reference value is a screening tool to identify children with higher levels of lead in their blood compared to most other children and initiate care. It is NOT a lower threshold for lead poisoning in children.
It is a statistical value based on blood lead values among US children ages 1-5 from the most recent National Health and Nutrition Examination Survey (NHANES) cycles. The new CDC blood reference value is 3.5 micrograms per deciliter of blood (µg/dL), identifying the children with the top 2.5% of blood lead levels in the US. It is lower than the 5 µg/dL set in 2012.
The CDC reference value is neither health-based nor a regulatory standard. It presents guidance to physicians for recommending retesting and interventions to individual children based on their blood lead levels. According to the CDC, the following are the recommended actions:

Why lead is so destructive for children:
Although lead can harm adults, the primary concern today is with children since their developing brain is particularly susceptible to the adverse effects of lead. At very high levels, lead causes damage to the brain and nervous system, with effects including memory lapses, tremors, headaches, and stomach pains. There is no safe level for lead exposure in children. Even relatively low levels can cause adverse effects on the brain, including:
- Slowed growth and development
- Learning and behavior problems
- Hearing and speech problems
These problems can result in lower IQ, decreased ability to pay attention, and underperformance in schools.
How do children get exposed to lead?
Drinking-Water
As I have written, lead is found in drinking water due to lead pipes used in drinking water from the 1900s to the late 1980s. Although the EPA regulates lead in drinking water, there have been many incidents when lead has been detected in homes and schools, primarily due to the lead leaching from the pipes into the water.
Some cities have already taken action to remove lead pipes, and the recently signed infrastructure Bill contains money to remove existing lead pipes in the US. There needs to be a focus on removing the lead pipes as quickly as possible. It must not take another decade to get this done.
Soil
Lead occurs naturally in soil at very low levels due to its’ occurrence as an element in the earth’s crust. Higher concentrations can be found in contaminated areas
- near industrial sites
- roads in use before leaded gasoline was phased out
- around buildings that used lead paint that deteriorated as chips and dust. They can around new construction built on a site where an older home was torn down
Children are exposed to lead in soil through playing in the soil, breathing dust from contaminated soil, gardening, ingesting soil, and touching hands to mouth.
The good news is that it is relatively simple to get soil tested for lead today; inexpensive home test kits are available. However, it is rather difficult to interpret the test results. These tests are probably best used as an initial screening for lead in soil. For more accurate test results and information on interpreting the results, the Soil Science Society of America recommends several laboratories where you can get your soil tested for lead.
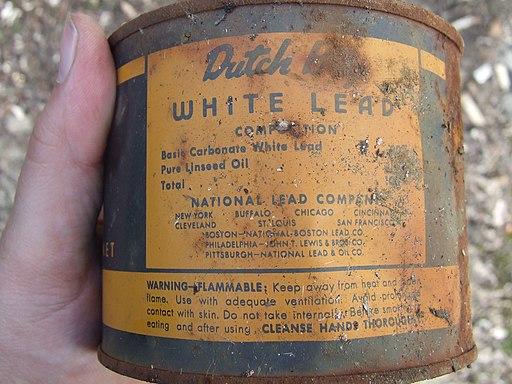
Paint
Lead-based paint was widely used in the US because of its durability. In 1978 Congress banned its use in residential structures.
 HUD and EPA have issued several regulations to reduce exposure to lead paint, including:
HUD and EPA have issued several regulations to reduce exposure to lead paint, including:
- The Residential Lead-Based Paint Hazard Reduction Act (1992)
- Lead-Based Paint Disclosure Rule (1996)
- Lead Safe Housing Rule (2004)
- Lead-Based Paint Renovation, Repair, and Painting Rule (2008).
These regulations have helped reduce children’s exposure to lead. However, lead paint remains a concern, particularly in older homes, buildings, and renovation.
What are the Trends?
Reducing environmental sources of lead has resulted in a reduction of blood lead levels in children. From 1978 to 2012, blood lead levels were reduced by 93%. This was due to regulations eliminating lead in gasoline which significantly reduced exposure through the air, and lead in drinking water, soil, paint, and consumer products.
But there are still too many children with elevated blood lead levels in the US. These children live primarily in lower wealth areas and housing built before 1950 - African-American children tend to have higher blood lead levels than White children.
The change in the CDC Reference Value Is Significant
Lowering the reference value is important. It means more children will be classified as at “high risk” and will result in more investigations of homes to identify potential sources of lead and address developmental issues.
But most clinical and office-based blood lead tests lack precision in measuring blood lead levels < 4 µg/dL. A study of 5 years of blood lead testing found that 40% of laboratories could not quantify blood lead levels of 1.48 µg/dL, and 23% reported limits of detection between 3 and 5 µg/dL. Measuring blood lead levels at or near the revised reference value will not be possible in a large number of cases.
Reducing lead exposure in children should not be dependent upon testing children for blood lead. Most neurological effects are very subtle, and when high blood lead levels are detected in children, it is usually too late to reverse the problem.
Conclusions
Lead is not a new issue; we have known about the health effects of lead for over 40 years. As a mom, I understand the heartbreak that can occur when your child’s health and development are at risk. I feel strongly that we need to do all we can to ensure children do not suffer the adverse effects of lead exposure.
It appears to me that that the CDC revised blood lead reference value is more of an academic exercise than a practical solution to bring about any real change in children’s lead exposure. To be effective, the revised blood lead level is dependent on greatly increased testing of children. As evident by the experience during the pandemic, this is not an area in which the CDC excels.
The way to solve this problem is not case-by-case, waiting to see if children have high blood lead levels. Instead, localities and local public health departments should take the lead and proactively go into the communities most at risk, i.e., older neighborhoods in industrial areas, and test for lead in soil, paint, and drinking water. This is a fundamental role for local public health departments that should be greatly expanded. Too often, in older neighborhoods, elected officials take an approach of “see no evil, hear no evil, speak no evil” instead of identifying, confronting, and resolving the lead issue.
[1] average test result in US children is about 1.4 µg/dL