The study utilized data from the Nurses’ Health Study (NHS) and the Health Professionals Follow-up Study (HPFS). The NHS contributed about 75,000 women, and the HPFS about 40,000 men. Participants completed surveys every two years regarding their medical history and lifestyle habits, with our old friend the food frequency questionnaire contributing information on their diet.
The participants’ diet was assessed every four years based on the NOVA food-processing classification [1], and the Alternate Healthy Eating Index (AHEI) was used to evaluate the diet's nutritional quality. In the initial analysis, alcohol was removed from consideration since it is “a well-studied risk factor for premature death and a distinct factor in diet;” whole grains with “established benefit for lowering all-cause mortality” were also removed from the initial analysis. The presence of a beneficial ingredient, whole grains, in food categorized as ultra-processed speaks to the inherent weakness of the NOVA classification as a nutritional discriminator.
The researchers considered the usual covariates available for review: body weight, smoking, and self-reported physical activity. Foods within each of the NOVA classifications were further subdivided [2]. The study outcome was all-cause and disease-specific mortality.
Participants with higher consumption of ultra-processed foods tended to be younger, less physically active, smokers, had higher body mass index, and lower AHEI scores, the measure of nutritional quality. [3]
“In two large prospective cohorts with up to 34 years of follow-up, we found that higher consumption of ultra-processed foods was associated with modestly higher all-cause mortality. We found no associations for mortality due to cancer or cardiovascular diseases.”
Modest indeed. Using a model looking solely at ultra-processed foods (UPF) and energy intake, those eating the highest amounts of UPFs had a 23% increase in all-cause mortality. However, adding in those other real-life variables, smoking, weight, and physical activity, the increase was now 4%, and the dose-response trend was lost when considering UPFs in isolation. UPFs are part of a lifestyle – at its simplest, those who are time-restrained may find UPFs are a more convenient diet in the same way those time constraints limit their exercise.
The findings of no association with cancer or cardiovascular disease suggest a more attenuated role of diet in the causation of these diseases, or to be fair, better attenuation through the use of statins and other medications. It also speaks to another “flaw” within the NOVA classification: red meat, the great Satan for some cancers, is not an ultra-processed foot; it is most often minimally processed.
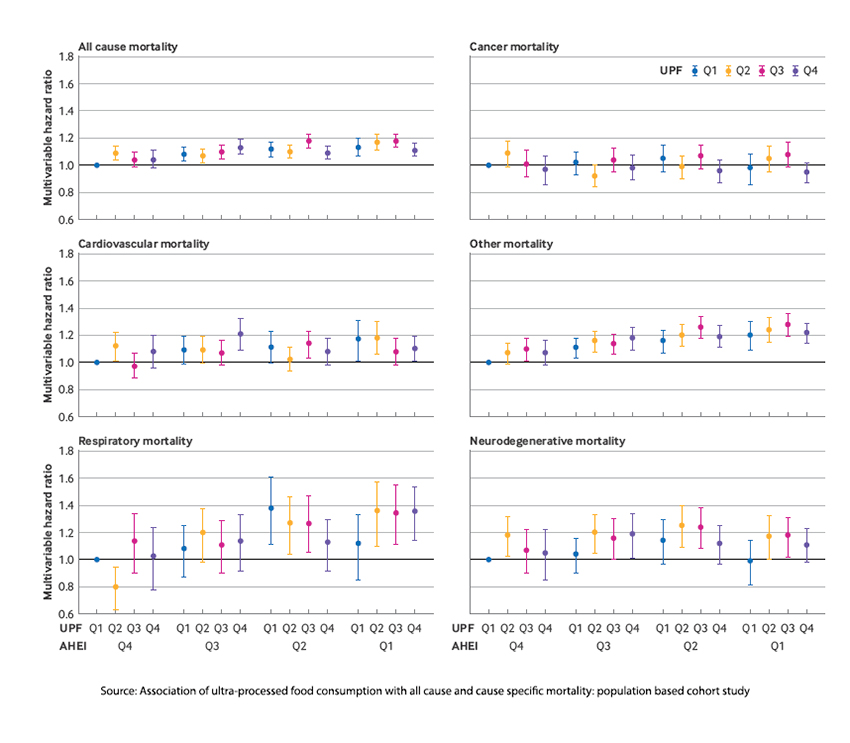
This graphic is a bit busy but shows the impact of UPFs and nutritional quality on mortality. For the AHEI (nutritional quality), Q4 has the greatest nutritional quality, and Q1 has the least. For the UPFs, Q4 are those eating the most ultra-processed foods. Those with the highest nutritional quality, AHEI Q4, and those who consume the least ultra-processed foods, UPF Q1, are the reference group. The researchers found that the nutritional quality of the food had a more significant impact on mortality than the amount of UPFs consumed within that category. In other words, it is not the UPF’s processing that is an issue, but their nutritional quality that makes a difference – and this is another reason why the NOVA classification, which is solely based on processing, is a poor measure in this and many other nutritional studies.
Another problematic point in the study, acknowledged by the researchers but more frequently ignored in media reports, was that adding back ultra-processed whole grains further weakened the association while adding back ultra-processed alcohol strengthened them. Again, it is not how a food is processed; mortality has more to do with its nutritional content, and even that is only a small factor when considering other lifestyle choices, including smoking and exercise.
Here is the researchers’ bottom line.
“Higher ultra-processed food intake was associated with slightly increased all-cause mortality. The mortality associations for ultra-processed food consumption were more modest than those for dietary quality and varied across ultra-processed food subgroups.”
They argue that avoiding those subgroups might be of value. For the curious, the one subgroup that stood out was ready-to-eat meat/poultry/seafood-based products. Runner-up were sugar-sweetened and artificially sweetened beverages, where sugar-sweetened had a more significant association with mortality than artificial sweeteners.
Contrary to the sensationalized narratives, these studies reveal a more nuanced reality. Higher consumption of ultra-processed foods is associated with a slight uptick in all-cause mortality, but the devil lies not in the processing but in the nutritional quality. Remember that moderation, balanced diets, and lifestyle choices are the true architects of our health destiny.
[1] The NOVA classification categorizes foods as unprocessed/minimally processed, processed culinary ingredients, processed foods, and ultra-processed foods.
[2] “ultra-processed breads and breakfast foods; fats, condiments, and sauces; packaged sweet snacks and desserts; sugar sweetened and artificially sweetened beverages; ready-to-eat/heat mixed dishes; meat/poultry/seafood based ready-to-eat products (for example, processed meat); packaged savory snacks; dairy based desserts; and other.”
[3] More specifically, they consumed less alcohol, whole fruits and vegetables, and whole grains.
Source: Association of ultra-processed food consumption with all cause and cause specific mortality: population based cohort study BMJ DOI: 10.1136/ bmj-2023-078476




