JAMA Internal Medicine published a sad, unsurprising study regarding hemodialysis (dialysis) in undocumented immigrants.
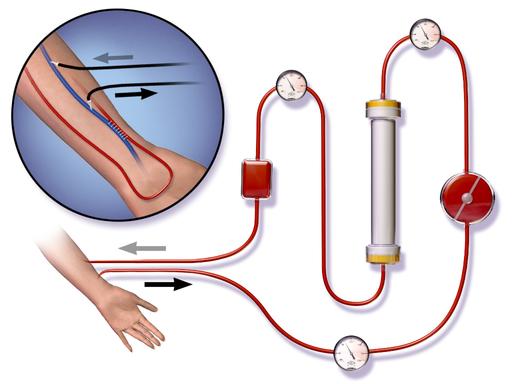
Let’s define a few terms so we can all be on the same page. End-stage renal disease is a condition in which your kidneys no longer function to clear toxins, which build up and cause a range of symptoms and death. We manage this problem primarily with dialysis, where the blood of the patient is cleansed of toxins continuously for about 3 hours. Unless there is some emergency reason, it is done three times a week and patients can be maintained this way for years.
The End-stage Renal Disease program, in which every patient in the United States ultimately is eligible, provides this care at reduced cost. [1] But obviously dialysis is costly and when the expenses are not paid, as is the case with people not in the country legally, the financial burden falls on hospitals as uncompensated care or on states through their taxpayer-funded Medicaid programs.
The paper is a limited retrospective review of care given in: two Texas hospitals, where dialysis for undocumented immigrants is provided on an emergency basis when toxins had built up to the point where they were symptomatic; one hospital in San Francisco where undocumented immigrants received standard dialysis 3-times a week and toxins never reached the symptomatic level. The total number of patients was small so generalization is not possible. Based on clinical parameters measuring nutrition (albumin) and oxygenation (Hemoglobin) those patients receiving emergency care will a bit sicker at baseline.
Additionally, nearly half of those patients had no prior care, in the US or their home country, so it is fair to say these patients were both more ill and less attended to than the patients receiving 3-times a week hemodialysis.
Clinical Consequences
Patients receiving emergency-only dialysis had
- Five-fold increase in 3-year mortality
- 14 fold increase in 5-year mortality
- Ten-fold increase in days in acute care (3 fold fewer days in office care)
compared with the undocumented immigrants receiving standard dialysis care. When compared with the overall end-stage renal disease patients the increased mortality was somewhat less at 2.2 fold higher.
What can account for these differences?
The authors looked at the overall mortality for the centers being studied. Both were low and the centers providing emergency-only dialysis actually had the lowest mortality in caring for their documented patients – so it is unlikely that the outpatient care differed.
The only difference in this limited study was that some patients had dialysis ‘as necessary’ and others received standard care.
States determine who receives emergency and standard dialysis when dealing with patients without insurance of any kind, which includes undocumented immigrants. Texas pays for emergency care, California for standard care.
Leaving undocumented immigrant status out of the equation, those receiving standard care three times a week care without any insurance did as well as insured patients; those receiving emergency care did worse.
As a physician I am held accountable for providing sub-standard care, do we, acting more anonymously as the state have a similar responsibility?
NOTE:
[1] It is a costly program 25 billion dollars in 2014 and guarantees that patients with end-stage renal disease become part of the Medicare program after a variable waiting period.
Source: JAMA Internal Medicine Association of Emergency-Only vs. Standard Hemodialysis with Mortality and Health Care Use Among Undocumented Immigrants with End-Stage Renal Disease DOI:10.1001/jamainternmed.2017.7039