The incidence of prostate cancer tripled between 1975 and the early 90’s. What changed? Sun exposure is an acknowledged risk factor in the development of melanoma – but oddly enough, for those with melanoma, a history of greater sun exposure is associated with a 50% better survival. How can sunlight be both good and bad? And women with higher socioeconomic status have twice the number of breast cancers diagnosed than their low socioeconomic status sisters. Does that mean that greater income somehow predisposes to breast cancer? How can all of these findings be true? Heisenberg.
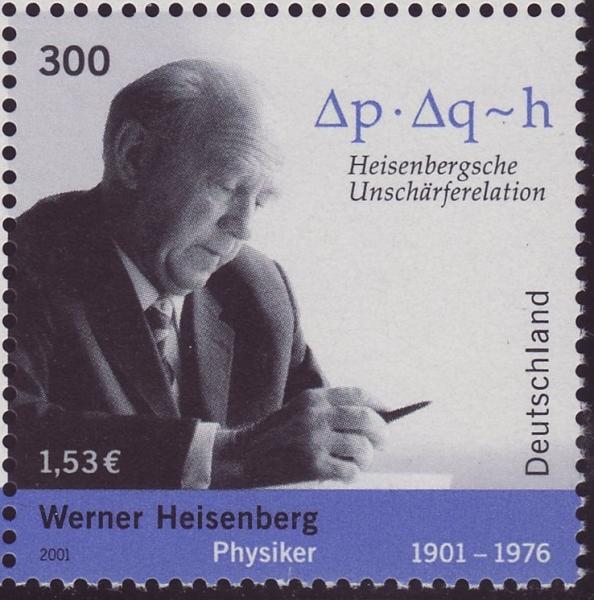
Werner Heisenberg and his ‘Uncertainty Principle’ are at play and are the subject of a thought piece on the uncertainty principle’s consequences for medical studies. The Heisenberg Uncertainty Principle states that the process of measurement changes what is being measured; you can never be entirely certain about both the measurement and the measured at once. How does this impact medical studies?
Increased scrutiny uncovers more cases
If you do not look, you rarely will find a problem. Screening for disease increases our searching, that is its purpose. The more cases we uncover, the more apparent the problem and the subsequent emphasis on more detection. Many articles demonstrating an increased incidence of disease more often a reflect our increasing search rather than some change in lifestyle or environment that is causing the increase.
Increase ability to detect small irregularities uncovers more cases
The poster boy for this has got to be prostate specific antigen or PSA. The big jump in prostate cancer was when screening went from a more uncomfortable and subject rectal examination to a more precise, less intrusive blood test. It is unlikely that something had changed in the water or that diet that caused the three-fold increase in prostate cancer, it was that scrutiny was now ‘on steroids.’ With more elevated PSA, we had more prostate biopsies, and more men faced the decision of whether to treat cancer we had found.
Because we were identifying these cancers earlier, we didn’t have useful information on how those cancers behaved. All of our knowledge, up to then, was based on cancers we could feel, not detect in a blood sample. Turns out, after several more years of study, and more men had to choose between observation, surgery or radiation therapy that many of those cancers found on PSA testing were slow growing and could be safely watched. The disease was different it was all not aggressive tumors it was a range of disease. Our more precise measurement, PSA, meant that prostate cancer was different than we had believed, it had changed.
The threshold for irregularity impacts cases identified
By lowering the threshold of concern, more cases appear – risking a dilemma of how to treat. Raising the threshold of concern and there are fewer cases – but outcomes change. Finding the sweet spot of thresholds is one of the purposes of guidelines. Fat and sugar have taken turns as the culprit for atherosclerosis. The shifting guidelines reflect Heisenberg’s “invisible hand” – scrutiny, more sensitive detection and a changing threshold for “abnormal” have altered atherosclerosis and its outcomes. It isn’t your parent’s disease.
Scrutiny determines populations which in turn identifies risk factors
The impact of measurement upon the measured can also explain much of the apparent disconnect between risk factors and disease and why a plausible biologic cause must underlie our thinking. Where is the credible biologic basis for higher socioeconomic status conferring a higher risk of breast cancer? Better food, environment or a genetic basis for wealth? It is not that higher economic situation is a risk factor, it is that higher economic status allows for more scrutiny, you can afford the testing. Sun exposure cannot plausibly simultaneously causes more melanoma and makes it more treatable. People with increased sun exposure will be scrutinized more often, or perhaps the cause of melanoma in that low exposure group is somehow different.
The uncertainty principle is alive and well in medicine; it explains some of the conflicting data and opinions that whipsaw public opinion. Heisenberg has much to say to physicians; we should make sure to share his insight more often in our public pronouncements and debate.
Source: Scrutiny-Dependent Cancer and Self-fulfilling Risk Factors Annals of Internal Medicine DOI: 10.7326/M17-2792