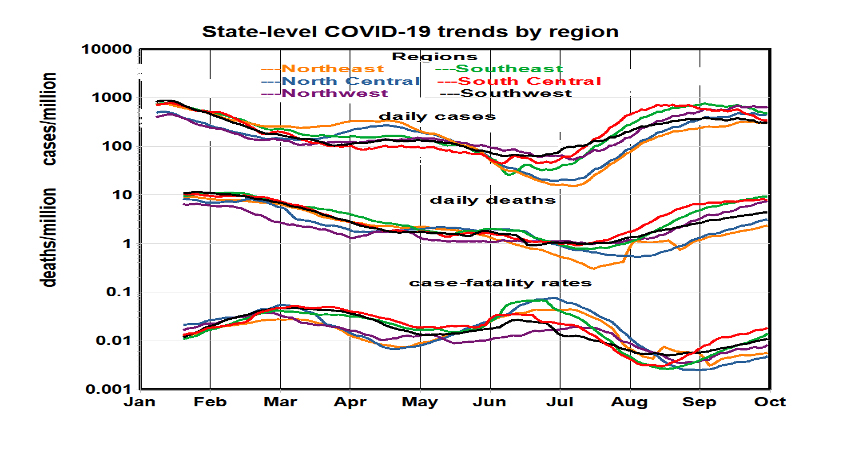
Trends in cases and deaths. The pandemic began in spring 2020 with the largest rates of infections in New York City and then spread throughout the nation, peaking in fall in the North Central region and in winter in the Southwest. The winter peak may have resulted from increased indoor activity and accompanying exposures. Vaccinations began in January with rates peaking in spring, but this period of relief was interrupted by the arrival and spread of the Delta variant. It appears that death rates may plateau next month. These trends are typical for all six regions within the US. Regional infection rates rank approximately in inverse order of their vaccination rates.
 Immunity and Risks. There are several ways to reduce populations at risk: mitigation, vaccination, immunity of survivors, and death. Mitigation strategies such as surface cleaning, face masking, and social distancing require continual implementation. Immunologic protection, acquired from the disease or by vaccination is longer lasting. The efficacy of the current COVID-19 vaccines has been demonstrated in both their clinical trials and subsequent statistical analyses of vaccinated populations. Vaccination is ostensibly “permanent” (thrice and done, including the current booster requirement). Immunity among COVID-19 survivors may vary with severity of the disease.
Immunity and Risks. There are several ways to reduce populations at risk: mitigation, vaccination, immunity of survivors, and death. Mitigation strategies such as surface cleaning, face masking, and social distancing require continual implementation. Immunologic protection, acquired from the disease or by vaccination is longer lasting. The efficacy of the current COVID-19 vaccines has been demonstrated in both their clinical trials and subsequent statistical analyses of vaccinated populations. Vaccination is ostensibly “permanent” (thrice and done, including the current booster requirement). Immunity among COVID-19 survivors may vary with severity of the disease.
Immunity acquired through infection with COVID-19 can be an important public health consideration but only pertains to COVID-19’s survivors, currently about 10% of the U.S. population. Vaccination applies to a much large group. Vaccination rates peaked at about 0.5% per day and have since settled down to about 0.2% per day. Immunity from prior infection may be about 0.03% per day, based on current infection rates and assuming 98% survival. The current COVID-19 death rate is about 0.0006% daily.
However, only a small part of the general population is at risk on a given day. Assuming that about 10% of the population is vulnerable because of age or comorbidity and 10% of them are exposed to the virus, the actual population at risk would be reduced by a factor of 100, to 3.3 million. Mitigation strategies would be most cost-effective when focused on this subset, i.e., vaccination of the elderly and immune-compromised who tend to encounter crowded indoor spaces.
Comparison with Influenza.
Could COVID-19 become a tolerable “endemic” like seasonal influenza? if rates were no greater than for influenza? Mitigation strategies are measured as percentage reductions in rates of cases or deaths, but the associated public health objectives are posed in absolutes such as annual mortality counts. The answer lies with the criteria. The answer lies with the criteria.
The minimal annualized U.S. (pre-Delta) rates are about 4 million for cases and 670,000 for deaths. We don’t have annual or daily data for influenza but assume that seasonal totals are tantamount to annual. We assume  that October COVID-19 rates will persist for the year. Annual rates for infections are similar to influenza, but rates are up to an order of magnitude higher than influenza for more serious outcomes. The chart shows how difficult it may be to bring COVID-19 hospitalization and death rates in line with typical previous influenza rates; COVID-19 is a much more serious disease.
that October COVID-19 rates will persist for the year. Annual rates for infections are similar to influenza, but rates are up to an order of magnitude higher than influenza for more serious outcomes. The chart shows how difficult it may be to bring COVID-19 hospitalization and death rates in line with typical previous influenza rates; COVID-19 is a much more serious disease.
We used current data on daily vaccination rates to estimate rates of depletion of the population at risk and subsequent deaths under current conditions. Our estimates indicate that more than 2 years of increasing rates of vaccinations may be required to achieve acceptable rates of COVID infection and future variants may be likely during such an extensive period. The current considerable fraction of reluctant vaccinators poses an existential threat to achieving acceptable levels.
Some “what if” Scenarios. The 2021 data allow some generalizations and prognostications with respect to questions about the future:
- How many US lives may have been saved by vaccination from January to July? The median COVID-19 death rate has been about 3 per day per million population in summer, amounting to 178,000 deaths for the nation over the six months, about 25% of the total.
- Absent the Delta variant virus, how many additional lives might be saved with continued vaccinations? The death rate dropped by a factor of 10 after 56% full vaccinations. If 100% vaccination could be achieved, national deaths might be further reduced to an annual total of 20,000. COVID-19 death rates might approach those typical of seasonal flu if everyone were fully vaccinated. The median annual flu death rate during 2010-19 was 27,000.
- How many additional lives have been lost thus far due to the Delta virus variant? Mean daily death rates increased in August and September by about a factor of 10 from the median rate of 3 per million per day, about 60,000 more deaths for the nation.
What might have happened in the absence of vaccinations? - If the Delta variant had struck at the height of the winter peak when the mean COVID-19 death rate was about 10 per day per million, fatalities might have reached per million30 per day. Daily deaths across the US would have exceeded total annual US deaths from all non-COVID causes. The total mortality differentials recorded thus far are 178,000 lives saved from vaccination and 60,000 lost from the Delta variant. These hypothetical estimates range from less than influenza to greater than deaths from all non-COVID19 causes.

At this juncture, all the available mitigation strategies have been invoked: (surface disinfecting, social distancing, face masking, vaccinations), but population compliance has varied. Regional death rates now range over an order of magnitude, the largest of the year. Further progress depends on achieving more full vaccinations and avoiding new contagious virus variants.



