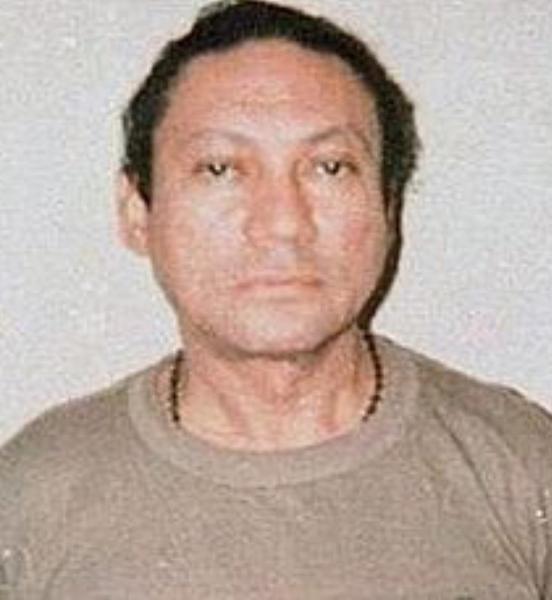
According to Reuter’s World News, “Panamanian former dictator, CIA spy and convicted cocaine trafficker Manuel Noriega was in a coma on Tuesday after suffering a hemorrhage from an operation to remove a benign brain tumor, representatives for the 83-year-old said.”
Here, we will address some basic tenets in neurosurgery (aka brain surgery) and how operating in this area of the body is often a delicate dance. It all comes down to real estate.
First, it is important to understand that tumors in the brain can be benign or malignant (aka cancerous). It is the location and ease of accessibility that dictates the level of surgical resection complexity. A benign tumor tickling the brain stem, for example, could be more precarious than a low grade malignant one in a more superficial spot where not a lot of high executive function and judgement, for instance, takes place. The brain stem is critical to controlling our basic ability to breathe on our own and maintain consciousness. Injury to it can be catastrophic.
Why remove a benign tumor? These have a tendency to grow over time. If one has gotten so large that it is impacting vital neighboring structures, then a patient can become increasingly symptomatic with seizures, severe or persistent headaches, vomiting, vision or sensory and personality changes, dizziness, confusion and coordination impairments to name a few. Furthermore, for these reasons along with any associated inflammation, they do most of their harm by mass effect (aka the displacing of surrounding tissue).
To learn more about tumor differences, then review my two-part series where I interview Dr. Gregory Riggins, Professor of Neurosurgery and Oncology and Director of the Brain Cancer Biology and Therapy Research Laboratory at Johns Hopkins: Brain Tumors: Fact Vs. Fiction—Part I and Brain Tumors: Fact Vs. Fiction—Part II.
Rheuter’s continues and reports, according to his daughter Lorena Noriega— who spoke with reporters by Santo Tomas Hospital where he had his surgery— he is “critical” and “He has a major brain hemorrhage and is in serious condition.”
“Brain hemorrhage” (aka a bleed in the brain or a form of stroke) is unfortunately a potential outcome of high risk brain operations, in general. They may result from trauma or those with especially weak blood vessels. Those who abuse drugs, in particular cocaine. Here, Noriega’s lawyer, Ezra Angel, indicated “high blood pressure may have contributed to the hemorrhage.” High blood pressure is a big culprit in causing these types of complications.
Blood pressure is of significant importance when managing brain surgeries. Too low, then the brain is inadequately perfused and deprived of oxygen. Too high, and this type of bleeding injury can occur. Because brain cells don’t regenerate like peripheral nerves can, damage is done and determined by extent and location. The central nervous system is the command center for regulating this crucial vital sign. To learn why it is so substantial a metric, read Do Vital Signs Wrong and Pay Ultimate Price.
As per Angel, Noriega “underwent a second operation that stopped the bleeding” and “the second operation in eight hours was carried out with "open skull” adding that his client was in an induced coma.” When an individual has a surgery to remove a brain tumor, they are closely monitored afterward to observe for signs of a bleed in the head. If those appear, then another surgery is often required to correct the problem.
The brain— with its vessels properly encased—likes to be left alone as nature intended. When something is where it shouldn’t be albeit a tumor or blood, the brain gets irritated. Inflammation ensues. And swelling. Imagine how much space there is for the brain to swell against an enclosed skull? A very limited amount.
So, what happens in such situations if the skull is not opened and that pressure released? The brain has nowhere to go and can herniate on the brain stem. Death can be inevitable.
Controlling and monitoring intracranial pressure is extremely important in any neurosurgery. Fortunately, there are ways to control it that involve medications and less invasive procedures, but when circumstances become more extreme surgery is required. Inducing comas is a measure frequently employed to stabilize these processes.
Additionally, there are post-surgical considerations that must be aggressively incorporated into doctors’ treatment plans. To learn more about surgical complications and efforts to avoid them, read Bill Paxton Dies of Surgical Complications.
When it comes to surgery, in general, the absolutely most pristine operation can take place and a complication still arise. People are complex as are their underlying diseases and variations. The perioperative period can be especially perilous when dealing with the most premier real estate like the brain or heart. Fortunately, we know what to look for and how to intervene to prevent progression. For many with bad disease, however, it can be the best option and their only hope. Each person is different in terms of degree of illness, medications used, medical or family history, resilience and reserve etc… so the same procedure needs to be weighed against his/her personal risks. Always discuss these with your own doctor who knows you and your comprehensive history and physical examination.