We all know the basics of healthy living, eat right, get enough sleep, move around. But it can be hard to get enough sleep if your homeless, tough to eat right if you live in a “food desert,” and well, at least you can move around. So, it should be no surprise that there is an effort to make these healthful basics a part of healthcare; they are the social “determinants.” Whether hospitals and healthcare systems are the right agencies to dispense these social determinants is beyond the scope of what I am writing. I’ll just remind you that the Children’s Hospital of Philadelphia open a McDonald’s in the hospital over 30 years ago and that Cleveland Clinic has a Holiday Inn right on its campus to accommodate patient families – you decide.
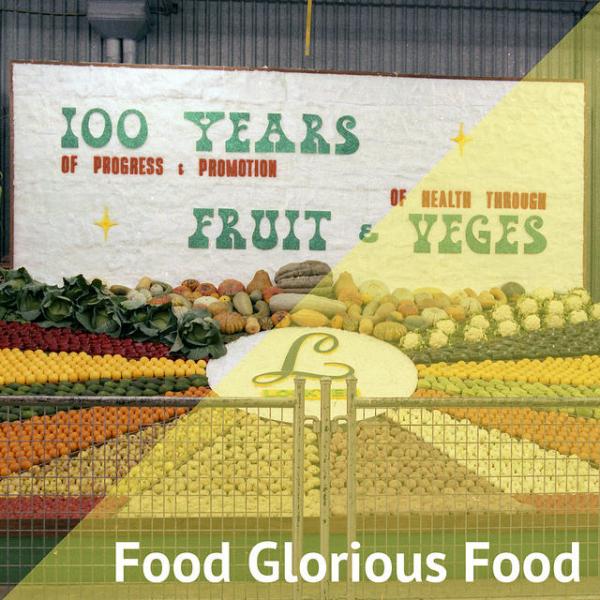
Two recent articles address getting nutritious food to those in need, as a healthcare prescription.
The first is an economic analysis looking at a 30% subsidy for fruits and vegetables or a 30% subsidy for fruits, vegetables, whole grains, nuts/seeds, seafood, and plant oils for Medicare and Medicaid beneficiaries in improving their health. Their results were based on a model predicting cardiovascular disease and diabetes based on established risk factors including diet. The details are unimportant, they made a good faith effort, and we can always quibble about the results. Not surprisingly, for both scenarios, the money expended on funding and administering the program was eclipsed by the additional individuals who did not develop cardiovascular disease or diabetes or where the natural course of these diseases was altered to make them less onerous.
- A subsidy for fruits and vegetables, increasing consumption by only a half serving daily, resulted in a savings of roughly $40 billion over about 18 years.
- Adding the additional subsidy for whole grains, nuts/seeds, seafood, and plant oils increased consumption by a quarter serving daily, resulted in a savings of about $100 billion over the same period.
These calculations are tempered by the authors, “Our model cannot prove the health and cost effects of these food incentive programs…. the estimates provide evidence that can be considered and incorporated into the design and evaluation of incentive programs…” What I do know of these programs is that costs are real, and the presumptive benefits and savings are sometime in the future.
In the fruit and vegetable only scenario, the model predicted that more people not less developed diabetes. That was because there was no data for fruits and vegetables preventing diabetes - as a result, more people survived cardiovascular disease but then hung around long enough to develop diabetes. Like Whack-a-Mole if you survive one disease another will get you, no one so far has eaten so well as to avoid dying. Here is Medicare’s breakdown for other chronic conditions, the ones in the red box are accounted for by the model; but depression, chronic kidney and pulmonary disease, and cancers are not, and they will remain expensive and will be more likely to develop as we reduce those cardiovascular deaths.
 I am not advocating that we do nothing, just that the costs may be a lot greater.
I am not advocating that we do nothing, just that the costs may be a lot greater.
The second study, meant to be a pilot just like the first paper, was an observational study on improving food choices. The study was conducted in a food pantry, where individuals could come in monthly and freely select foods they and their family needed and chose to eat. The study foods were kale, whole-wheat pasta, and brown rice, all part of a healthy diet and at baseline infrequently selected. The control scenario, these products were just on the shelf just like in a supermarket. A local chef designed a meal using those ingredients personalized to the neighborhood. In one trial, a sample of the meal was provided along with a recipe; and in the other trial, in addition to the sample and recipe, the ingredients were already bundled together.
They chose these ingredients three times more often when they had a chance to taste a dish, get a recipe and the ingredients were conveniently bundled and ready to go. Just tasting a recipe was nice but it didn’t move the needle.
This study has its flaws too, but again we are looking for opportunities here not truths. Aside from the cost of consulting with a neighborhood chef and vetting the idea within the community the cost of the program was pretty low; making a few meals and recipe cards.
Let me pose a question. Of these two pilots, which should we prioritize? A simple, neighborhood-based nudge or a large federal program dangling a subsidy that will attract special interests. Which program is more empowering for an individual, one that teaches what to do with kale and a can of beans or one which hands you a price reduction and wishes you well?
Sources: Cost-effectiveness of financial incentives for improving diet and health through Medicare and Medicaid: A microsimulation study PLOS Medicine DOI: 10.1371/journal.pmed.1002761
Ingredient bundles and recipe tastings in food pantries: a pilot study to increase the selection of healthy food Public Health Nutrition DOI: 10.1017/S1368980019000259