In 2013, the American Heart Association (AHA) and the American College of Cardiology (ACC) created a “risk calculator” to estimate the 10-year risk of atherosclerotic cardiovascular disease (ASCVD) and guide patient-centered medical therapy for prevention strategies, like starting statins. However, concerns arose that the pooled cohort equations (PCEs) overestimate risk and do not reflect the current diverse US population, particularly underrepresenting Asian and Hispanic adults.
In 2023, AHA's Cardiovascular-Kidney-Metabolic Scientific Advisory Group introduced a new “calculator,” the Predicting Risk of Cardiovascular Disease Events (PREVENT) equations. These new equations reflect more diverse and recent cohorts from electronic health record data.
Because of differences in the risk factors considered, the composition of the patients studied, as well as the significant changes in preventative care during the 40+-year breadth of studies incorporated into these risk calculators,
“Adoption and implementation of the PREVENT equations could substantially lower multiple domains of preventive medication use, particularly among older adults.”
To arrive at this conclusion, the researchers looked at participants in our old friend, the National Health and Nutrition Examination Survey (NHANES), to contrast the impact of these two calculators on “estimates of 10-year ASCVD risk and recommendations for primary prevention statin therapy across the US adult population and in key demographic groups.”
The “weighted study sample” of 3785 participants had no prior history of cardiovascular disease. Individuals with missing laboratory data were excluded, and the age range of 40 to 75 years was used to mimic the population subject to these risk calculations in primary preventative care. The mean age was 55.7, slightly more females than males. White participants were slightly over-represented, primarily to the detriment of under-representation by Hispanics. There was a greater percentage of individuals with diabetes and current smokers, with a lower percentage of individuals taking statins
The 2019 ACC/AHA guidelines for the primary prevention of CVD recommend statins for individuals with
- Diabetes
- LDL of greater >190 mg/dL
- An estimated 10-year ASCVD risk of >7.5%
Those with calculated risks below 7.5%, low or borderline, do not routinely receive a recommendation to begin statins. Calculated values up to 19.9% are considered intermediate risk, and greater values are considered high-risk patients.
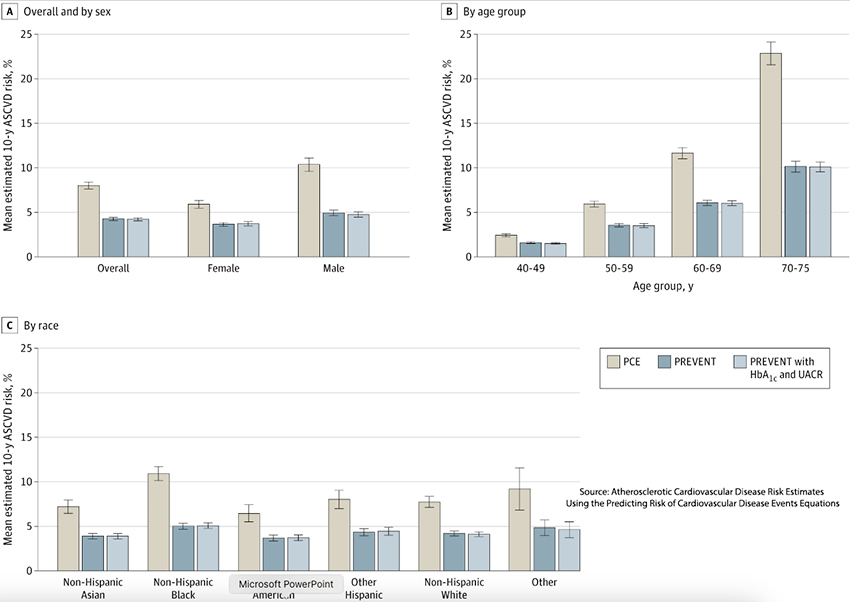
- Across all age, sex, and racial subgroups, the PREVENT calculation was lower than the older PCE calculator. The largest differences were for Black individuals and adults aged 70-75.
- Among those that PCE considered at intermediate risk, PREVENT 71% at low or borderline risk, and only 0.1% were reclassified as at higher risk.
- Among those that PCE considered at high risk, PREVENT classified 94% as intermediate risk and 2.3% as borderline risk.
- These risk adjustments were consistent across all ages, genders, and races.
Applying current AHA recommendations utilizing PREVENT over PCE would result in
- 38% of adults, 17.3 million, would no longer be recommended statins (including 4.1 million currently taking statins).
- 0.2 million would be newly recommended statins
- While these shifts were similar for gender and racial groups, there were larger shifts away from statins in those 50 to 69 years of age.
It seems that, like aspirin's role in preventing heart disease, statin’s days as THE preventative treatment for heart disease may be numbered. While reducing statin use among those no longer “at risk,” at least according to PREVENT, would represent a savings to many, including those out-of-pocket costs, as the researcher note,
“Deimplementing statins for the 4.1 million adults in the US who would no longer meet ASCVD risk criteria but currently take statins could be more challenging, with the potential to lead to patient confusion over shifting recommendations, particularly as many adults at borderline risk of ASCVD may again reach statin eligibility after a few years.”
Before rushing out to be deprescribed, it is essential to note that even the researchers cannot “tell which risk score is more accurate in today’s practice, making the overall risk and benefit of the changes uncertain.”
That uncertain comes from limitations on the data they used; this iteration of NHANES had less than a 50% response rate, making its reflection of our habits unclear; in some of their treatment assumptions, other groups recommend a higher or lower risk % for advising statins; and additional considerations, like family history, that make personalize medical treatment genuinely personal.
Why are the calculations so different?
The most obvious reason is that different variables and patient populations were used in their development. PREVENT added a measure of kidney function “in recognition of the link between cardiovascular, kidney, and metabolic health.” The current use of statins was added because they appear protective, and the data used in developing PCE was older before they were commercially available.
PREVENT did not consider race; PCE considered individuals Black or White. [1] The researchers, in discussing dropping the variable of race, write,
“The removal of race reflects the growing consensus of race and ethnicity as social constructs and the reconsideration of current clinical tools to ensure these constructs do not perpetuate inequities in clinical care.”
There is quite a bit to unpack there, and it is better to leave it for another day. But certainly, it may help to explain the lowering of risk for patients self-described as Black.
The underlying patient data was also different. PREVENT utilized more contemporary billing and electronic health record data, a two-edged sword. As the researchers note
“These data sources are much larger and more recent than the cohorts that constituted the PCEs, making it possible that PREVENT is recognizing a true change in risk. But electronic health record data are also more prone to error.”
One of the lessons from COVID is the dynamic nature of communicable, infectious diseases. This study clarifies that there are dynamic changes to non-communicable diseases, like heart disease, but their prolonged time frame may mask those dynamics. Our guidance in best caring for our health and the calculations and calculators underlying that guidance will never be one-and-done, and the changing recommendations are not flip-flops but a recognition that everything evolves, including the diseases that afflict us and their treatment.
Our understanding of cardiovascular risk and prevention is far from static. This evolving landscape underscores the need for continuous adaptation in our approach to heart health.
[1] NHANES uses a different categorization of race, and the researchers collapsed all participants except non-Hispanic Blacks, such as Whites, in their calculations of the impact of the PCE calculator. PREVENT replaces race with zip code.
Source: Atherosclerotic Cardiovascular Disease Risk Estimates Using the Predicting Risk of Cardiovascular Disease Events Equations JAMA Internal Medicine DOI: 10.1001/jamainternmed.2024.1302




