
The US Environmental Protection Agency (EPA) recently announced grant financing to improve indoor air quality (IAQ) in 5 school systems. They noted that about half of US schools do not have “indoor air quality management plans or programs in place.” Such plans focus on windows and HVAC systems, adopting the EPA policy of addressing indoor emissions separately from outdoor air pollution. The 2008 EPA IAQ guide does not mention population exposures from ventilating with outdoor air; it’s almost as if indoor and outdoor air pollution are the concerns of different agencies. Here is my alternative.
Background
Routine monitoring of US outdoor air quality began in the 1950s, considering several vital characteristics: toxicity, time histories, and spatial distributions. Toxicities have been established for regulated (outdoor) pollutants but not for common household sources such as cleaning, air fresheners, pets, or insecticides, for which data on time histories and spatial distributions are scarce. It is axiomatic that definition must precede regulation; we can’t control what we don’t understand.
The published literature on IAQ is voluminous. [1] However, most of the literature focused on exposures rather than health outcomes. The epidemiology of IAQ is quite sparse, partly due to difficulties in obtaining samples large enough to achieve statistical significance. Additionally, the outside air was so dirty in the 1950’s that indoor air didn’t matter. The EPA was primarily tasked as a regulatory agency with reducing institutional and vehicular emissions, which has largely been accomplished. Today’s pollution sources are in our 127 million households.
Air quality controls intended to benefit the health and well-being of residents are based on ambient measurements at selected outdoor locations. Current (outdoor) air pollution control strategies are based on the EPA's “no-threshold premise,” i.e., that even the lowest concentrations can be harmful. However, actual population exposures tend to be much more heterogeneous, even within households. For example, the presence of a single cigarette smoker has been estimated to double indoor particulate levels.[2]
Indoor vs. Outdoor Air Quality
There are important distinctions between outdoor and indoor air pollution.
- Control of outdoor air pollution is limited to defined emission sources operated by “them,” i.e., vehicular traffic, electric power generation, manufacturing, mining, and agriculture. By contrast, indoor air quality is controlled by individuals, i.e., us.
- Outdoor air quality responds to weather fluctuations in the short term measured in days. The worst episodes have been caused by widespread prolonged periods of air stagnation. By contrast, indoor air pollution is controlled by individual activities, including smoking, cooking, cleaning, pets, candles, and fireplaces. While these sources vary considerably by household and within communities, they tend to remain stable over the long term, as measured in years.
- Not all pollutants are found both indoors and outdoors. Radon gas, a concerning carcinogen, is
found mainly indoors, where concentrations may be reduced by opening windows. Ozone is formed by atmospheric chemical reactions and has no indoor sources.
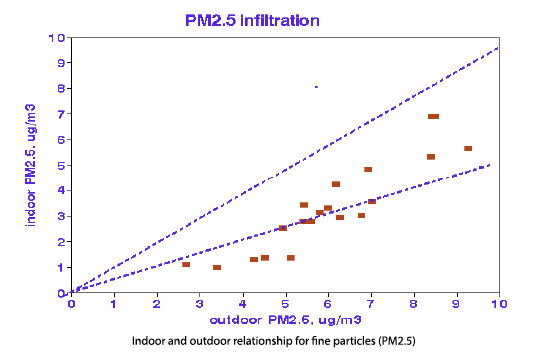 Ventilation merges these two contributions to IAQ; about half of outdoor contamination infiltrates indoors. Advice about opening windows to improve indoor air quality should thus be conditional. In a tightly sealed structure, indoor pollutants may unduly impact residents irrespective of outdoor pollutants. In structures more open to outdoor sources, outdoor pollutants may play a greater role.
Ventilation merges these two contributions to IAQ; about half of outdoor contamination infiltrates indoors. Advice about opening windows to improve indoor air quality should thus be conditional. In a tightly sealed structure, indoor pollutants may unduly impact residents irrespective of outdoor pollutants. In structures more open to outdoor sources, outdoor pollutants may play a greater role.
Personal Exposures
Concerns about individual exposures were expressed early on but have largely been ignored by the epidemiology community, reflecting the difficulties with obtaining the required exposure data rather than in recognizing the need. Epidemiological significance requires hundreds of subjects over extensive periods.
Conventional epidemiology studies compare group outcomes, such as mortality rates, with air quality measurements from centrally located monitors. However, indoor exposure data must be obtained from individual residences, and personal exposure data must be obtained for each resident.
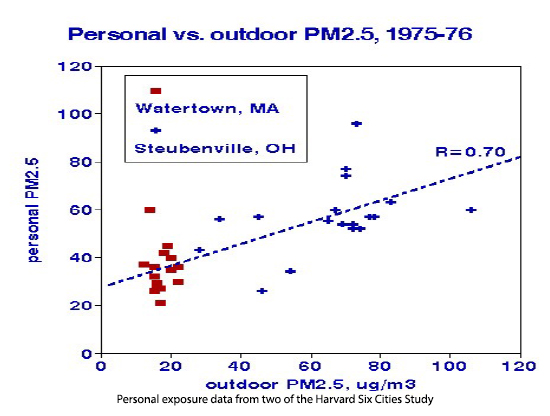 This graphic shows important differences between two cities. Watertown is mainly residential, and personal PM2.5 varies 3-fold and exceeds outdoor levels. Steubenville is heavily industrial; indoor concentrations vary 4-fold, loosely related to the outdoors. The overall personal/outdoor relationship results from differences between rather than within the 2 cities.
This graphic shows important differences between two cities. Watertown is mainly residential, and personal PM2.5 varies 3-fold and exceeds outdoor levels. Steubenville is heavily industrial; indoor concentrations vary 4-fold, loosely related to the outdoors. The overall personal/outdoor relationship results from differences between rather than within the 2 cities.
A more relevant personal exposure study followed 178 residents of Riverside, California, in 1990. PM levels from monitors attached to individuals, their personal “clouds,” were about 50% higher than indoor or outdoor levels. Such clouds were not reported for CO or NO2, and indoor PM concentrations were only weakly correlated with outdoor levels. Particulates are the most important pollutant in that concentrations and exposures may be substantially higher in the immediate vicinity of individuals than elsewhere in the room. Such differences vary among individuals and pose substantial barriers to effective epidemiology.
What’s To Be Done?
It seems irresponsible to monitor and regulate outdoor air while ignoring similar indoor concentrations. Are these low concentrations harmful or not? EPA predicts thousands of premature deaths associated with these low mean outdoor levels. We need to:
- Determine Toxicities of Indoor Pollutants Indoor air pollution sources are diverse, especially for particulate matter (PM). Risk assessments have been based on total PM mass regardless of composition, resulting in substantial uncertainties in estimated health risks. However, indoor sources can be grouped into a manageable number of categories, such as smoking, combustion including gas stoves, dust, cleaning products, and pet dander.
- Collect Data Buildings are required to operate CO and smoke alarms; why not similar requirements for PM2.5? Low-cost instruments are available, and ultimately, alarms could signal harmful levels.
- Base Short-Term Risk Assessments on Infiltrated Outdoor Air With 50% of indoor infiltrated from outdoors, the highest indoor exposures may occur during weather-related exacerbations of outdoor pollutants. Risk estimates based on more exact indoor concentrations would be more accurate.
- Focus Regulations on Short-Term Peaks Rather Than Long-Term Means Mortality risks based on short-term episodes have been supported by body counts and autopsies. There is no such supporting evidence for regulated long-term averages. Regulations should focus on achieving 24-hour standards, which PM exceeded only 9 times in the US in 2023.
- Revisit Air Pollution Control Strategies Improved air quality requires reduced emissions, so what’s new here? The key should be data-centered individual control of exposures. As proclaimed by Paracelsus ca. 1500, “The dose makes the poison.” In the case of indoor pollution, we, the people, make the doses.
Regulatory agencies face alternative ways to deal with indoor air pollution, each with significant consequences. Persisting in only measuring outdoor pollutants, when we spend 85% of our time indoors, and 50% or less of outdoor pollutants find their way indoors, will produce negligible health benefits. Basing public health risk assessment on peak indoor exposure will reflect our personal exposures more accurately and allow us more control. The EPA grants should be based on collecting data.
[1] The National Library of Medicine listed 18,372 publications containing the terms “indoor air quality” or “indoor air pollution,” adding “outdoor” to the search criteria reduced the number of publications to 3168, restriction to the US yielded 544, and adding “ventilation” reduced the list to 123. A separate search for “personal” air pollution exposure studies produced 17 citations.
[2] Estimated distributions of personal exposure to respirable particles. Environment Monitoring Assessment DOI:10.1007/BF00394173


